Yiyuan Zhao1 (RN,MSN,NP), Jingjing Wang1 (RN,BN), Yanli Wang2(RD), Yening Zhang3(MD), Ying Zhang1(RN,BN), Bin Zhang1(MD,Professor), Yuhan Lu4(RN,MSN,NP, Professor)
1. The Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Head and Neck, Peking University Cancer Hospital & Institute, Beijing, China
2. The Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Nutrition, Peking University Cancer Hospital & Institute, Beijing, China
3. The Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Psycho-oncology, Peking University Cancer Hospital & Institute, Beijing, China
4.The Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Nursing Department, Peking University Cancer Hospital & Institute, Beijing, China
Rehabilitation management is crucial for postoperative inpatients with head and neck cancer (HNC) to reduce treatment related complications such as excessive salivary flow, anastomotic fistula and poor nutritional status. Recently, we conducted a study that aimed to establish a Nutrition-Rehabilitation Multidisciplinary Team (NRMDT) led by nurses and evaluate the effects of adopting this model in rehabilitation management on improving clinical outcomes among patients with HNC.
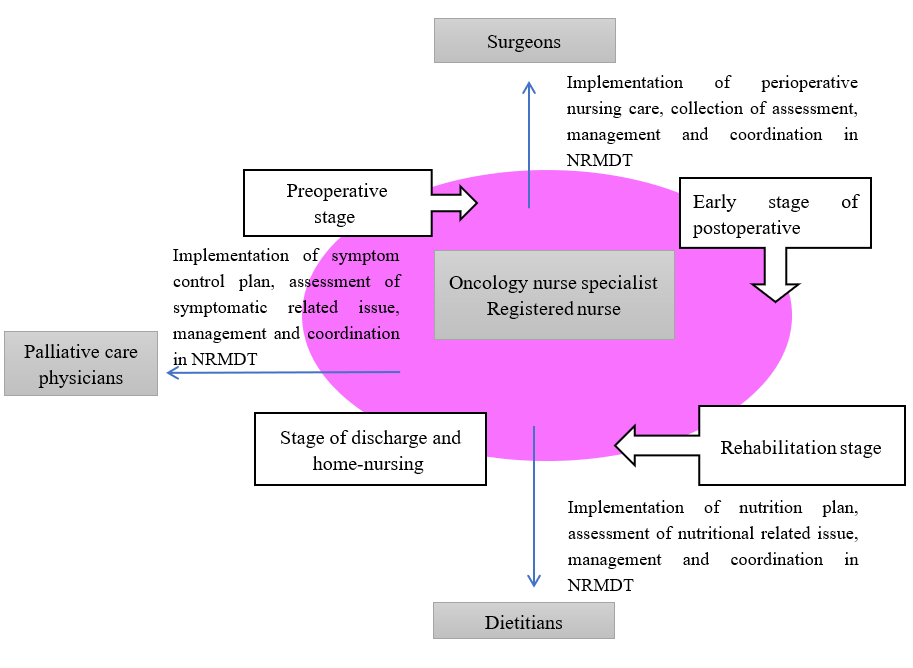
The NRMDT consists of a group of experts--surgeons, oncology nurse specialists, registered nurses, dietitians, palliative care physicians (Figure). The oncology nurse specialist in this department is also a certified Dysphagia Specified Nurse. The NRMDT is led by the oncology nurses who play essential roles in nutritional and symptom assessment, coordination of and monitoring multidisciplinary perioperative care (Table). They also provide a food-intaking-transition training to patients who have postoperative dysphagia (Picture).
Quasi-experimental design with a sequential sampling method was used in this study. The study was carried out from January 2017 to August 2021. A total of 49 HNC patients recruited were divided into the NRMDT group (n=38) and the control group (n=11). Patients in the control group received usual care from January 2017 to April 2018, whereas those in the NRMDT group were offered nutrition and rehabilitation management during the period of May 2018 to August 2021.Clinical outcomes including rates of weight loss, gastric tube dwelling time, the positive ratio of secretion, the occurrence rates of anatomic fistula, rates of hypoproteinemia, and length of stay were collected. SPSS software V.22.0 was used for data input and statistical analysis. Chi-square and independent-sample t-test were used to evaluate the clinical outcomes between these two groups.
The positive ratio of secretion in the NRMDT group was significantly lowerthan that in the control group(13.16% versus 45.45%, P=0.02). Furthermore, 2.63% of patients underwent anastomotic fistula in the NRMDT group, which was significantly lower than that in the control group (36.36%, P=0.01). The participants in the NRMDT group reported the proportion of weight loss and hypoproteinemia was 43.75% and 15.79% respectively, versus 54.54%(p=0.47) and 36.36% (p=0.29) in the control group. The days of gastric dwelling time and hospital length of stay were 16.87±7.91 and 19.89±6.31 in the NRMDT group compared with 21.18±9.87 (p=0.14) and 23.73±10.53 (p=0.27) in the control group.
This study demonstrated that the model of NRMDT may reduce the positive ratio of secretion and occurrence of anastomotic fistula among patients undergone surgery with HNC. A full‑scale study is warranted to examine its effects on improving other clinical outcomes for these patients.
Appendix
Figure The team members of NRMDT
Picture Assessment of dysphagia

Table Roles of nurses in the NRMDT model
|
Oncology nurse specialist
|
Registered nurse
|
|
Preoperative stage
|
Quality control and management of perioperative and multidisciplinary care
|
Assessment of symptoms and food/fluid intake and output, coordination of multidisciplinary care, and timely respond to patients’ needs
|
|
Early stage of postoperative
|
Quality control and management of perioperative and multidisciplinary care
|
Coordination of multidisciplinary care, provide post-operative care, timely respond to patients’ needs
|
|
Rehabilitation stage
|
Assessment of dysphagia, nutritional status, provide food-intaking-transition training to HNC patients
|
Implementation of oral intake/ nutrition plan designed by oncology nurse specialist / dietitian
|
|
Stage of discharge and home-nursing
|
Follow-up all the discharged cases in the online or face-to-face nursing clinic
|
Provision of general health education and evaluation (with other team members if needed)
|
This study was presented at ICCN2022 virtual conference.
Registration for ICCN2022 virtual library now open. For more information, please access https://www.iccn2022.com/registration/